Lesson objective:
In this lesson, we outline what happens in the amygdala, PFC, and the hippocampus during chronic stress.
We mentioned before that chronic stress affects the body, the brain, and our behavior.
And it should now be abundantly clear that chronic stress has profound and lasting effects on the entire body–across various systems.
While its structure and functions are in many ways unique from the rest of the body, the brain itself is also an organ, a part of the physical body. 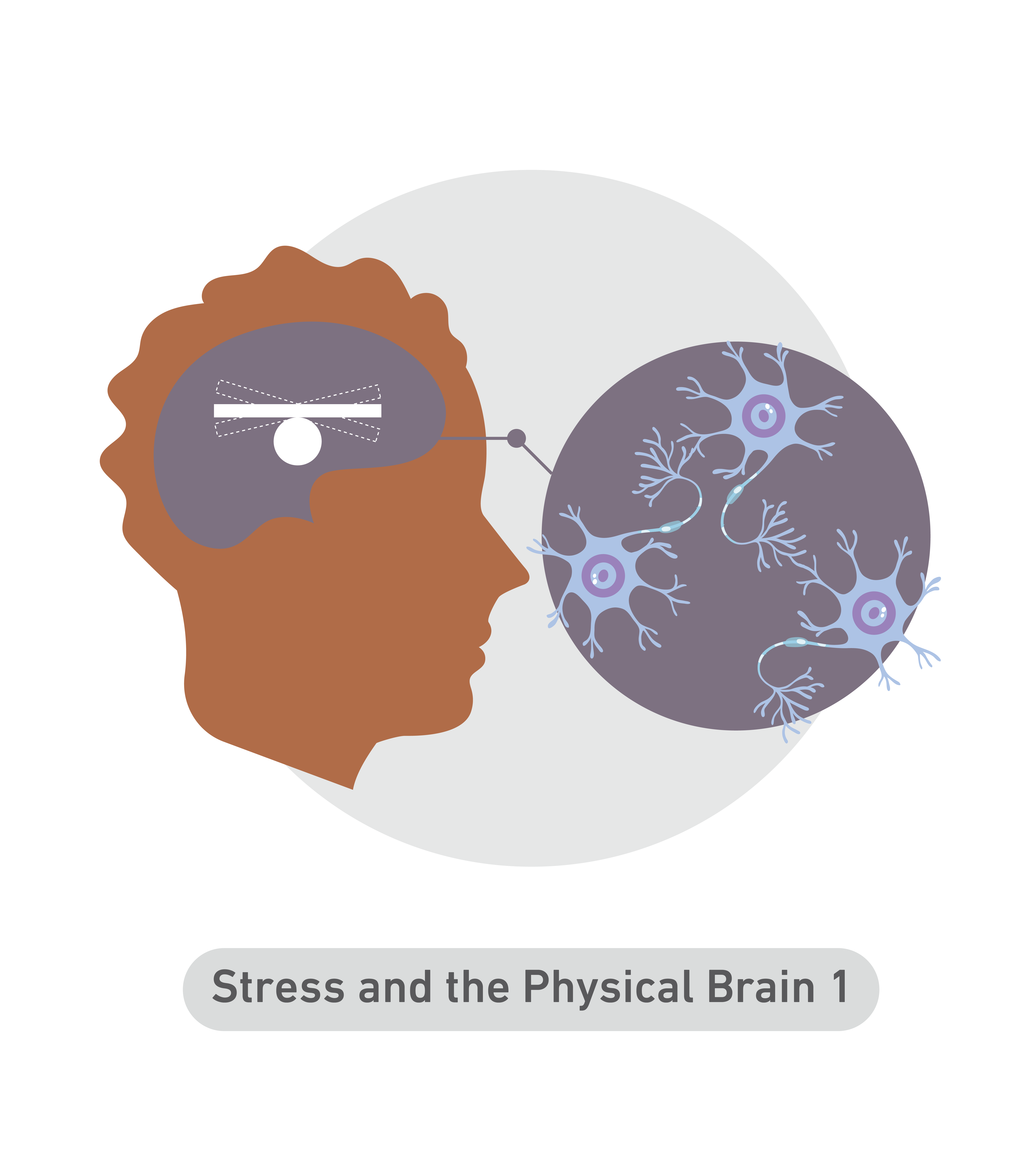
It is made up of water, fat, and trillions of neurons that occupy that space inside your skull. And just as other physical systems like the heart and lungs are affected by chronic stress, the brain as a physical organ is also affected.
Indeed, the physical brain changes due to chronic stress.
Chronic stress can affect both the physical size of certain parts of the brain and also the neural connections within and between those various parts. In other words, chronic stress affects the connection and communication pathways between neurons, affecting thoughts, emotions, and abilities.
While the stress process enlists the whole brain, there are three regions that are particularly affected by chronic stress. These three regions are the hippocampus, the amygdala, and the prefrontal cortex.
Chronic stress can affect the physical shape, size, and connections in these areas through three separate processes:
First, dendritic retraction and branching. This just means that individual neurons shrink in size, and the number of connecting “branches” they have decreases or increases.
Second, synapse
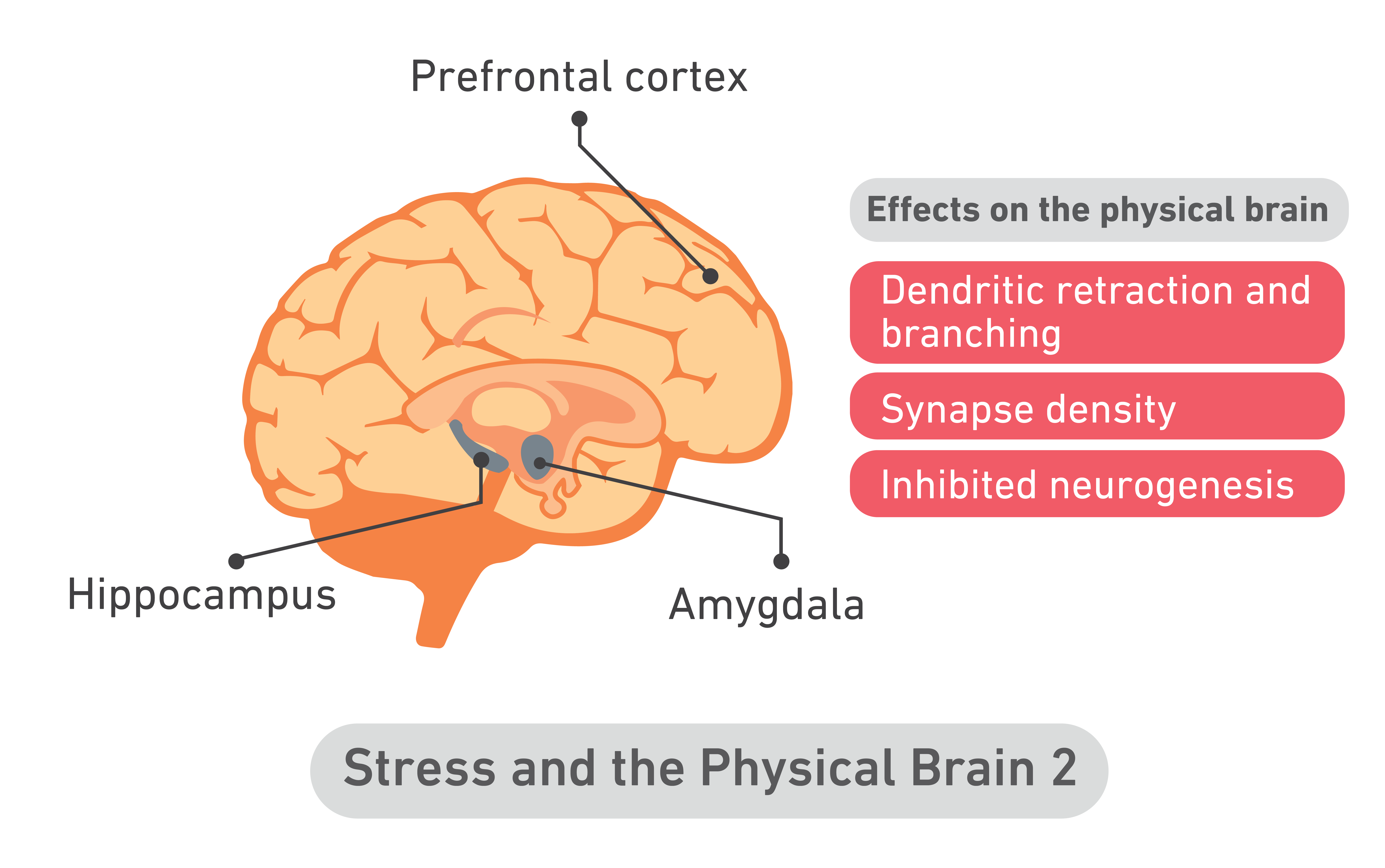
density. This refers to the density of synapses–the functions of communication–in a given region of the brain.
And lastly, inhibited neurogenesis. Simply, this is the inability of the brain to generate new neurons and neuronal connections.
So, let’s talk about the amygdala.
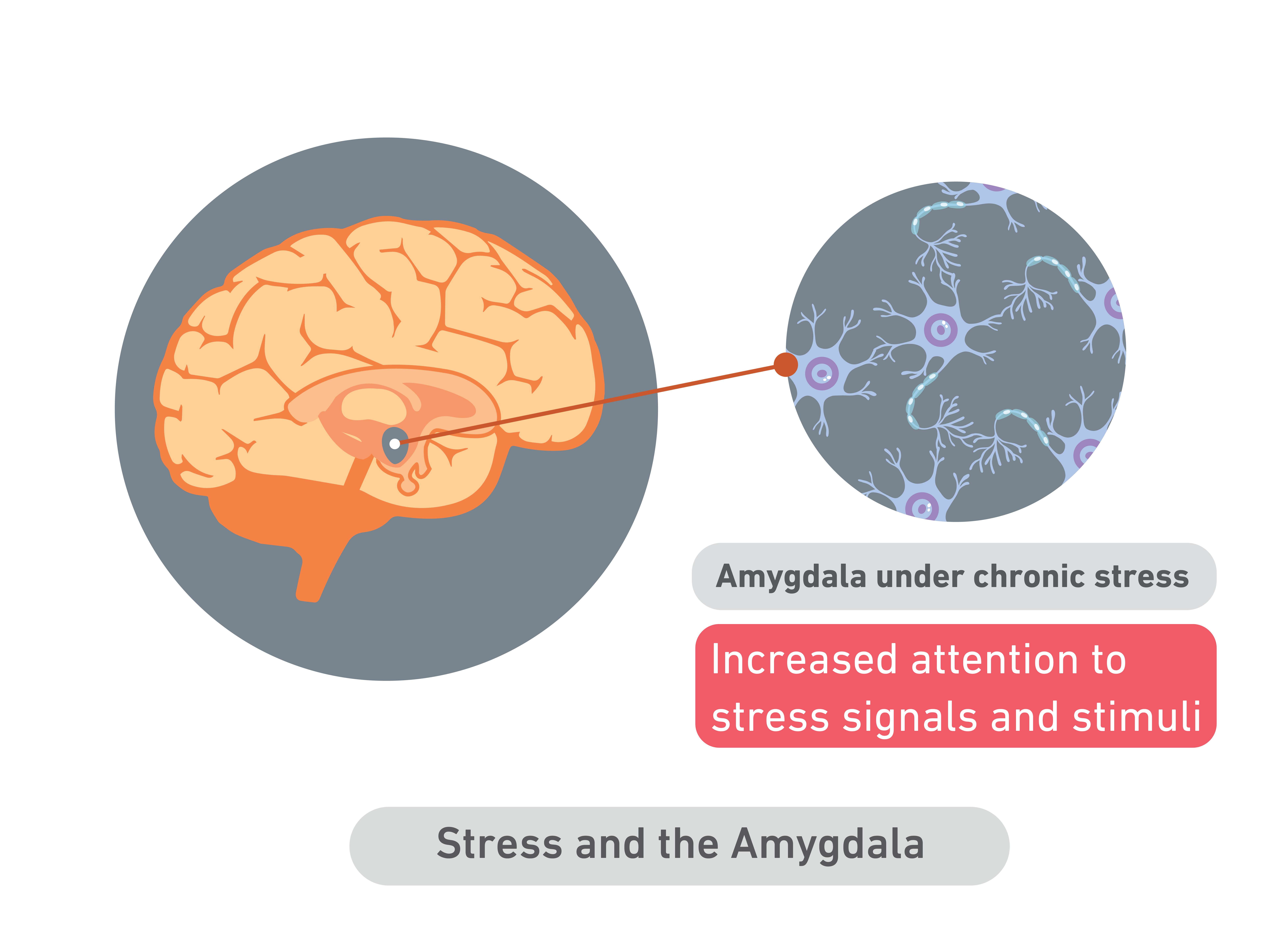
For example, chronic stress or fear can cause increased branching of neurons in parts of the amygdala. As we discussed, the amygdala serves as sort of an “alarm center” for the rest of the brain as the entry point and activator of the stress response. If your world is full of stress and potential threats, then it makes sense that the amygdala would increase its internal connections to be able to respond to this new demand. More connections means more communication, faster communication and mobilization.
Thicker neurons with more branches and connections can respond faster and better to an increase in stress signals. Thus, in people exposed to chronic stress, we often see an increase in size in the amygdala, caused by increased branching of neurons and the creation of new neurons.
In the short term, you can see how this expansion may be adaptive, as it allows you to pay more and closer attention to potential threats. Over time, however, elevated amygdala activity, or increased amygdala size, can encourage anxiety even when there is no real stressor present. As with many systems in the brain, what happens to the amygdala under chronic stress exposure is a short-term adaptive benefit that can turn into a long-term challenge, if the stress remains.
Second, let’s turn to the hippocampus.
We often see a decrease in neuronal density and branches in the hippocampus under conditions of chronic stress. This contrasts with what happens in the amygdala.
In times of sustained stress and threat, the hippocampus becomes overwhelmed
with information and conflicting signals from the adrenal cortex, the amygdala, and other contributors on the HPA axis. Thus, energy otherwise needed by the hippocampus is redirected to other parts of the body.
Research has shown that individuals who endure chronic stress can experience apical dendritic atrophy, a process in which a specific type of nerve cell called apical dendrites shrivel and stop working.
This occurs specifically in the hippocampus. In the experience of stress, apical dendrite branches degenerate. The loss of apical dendrites can manifest physically. It can often lead to significant weight loss and an increase in cortisol.
When apical dendritic atrophy takes place, the density of the hippocampus may be reduced; this can affect memory functions including remembering things like dates, names, and events, all the while reducing inhibitory signals of the HPA axis, thus making someone feel more stressed.
Simply, chronic stress interrupts key functions in the hippocampus. These key functions include the categorization and coding of emotions, and the encoding and retrieval of memories.
In other words, increased stress may affect your ability to retain new information, or remember information that you already “know,” as the hippocampus is either unable or too distracted to do so.
And finally, in the prefrontal cortex, we often see both neuronal growth and shrinkage.
The prefrontal cortex has many different functions and responsibilities, including analytical thinking, cognitive focus, self-control, emotion regulation, and sustained attention. It has many regions and sub-parts, and stress seems to target each area differently. Scientists are only just beginning to understand the effects of stress on the prefrontal cortex.
During times of chronic stress, the HPA axis exerts elevated influence over other systems in the body.
When stress hormones are elevated and the adrenal hormone system is hyperactive, neurons in many areas of the prefrontal cortex shrink. This neuronal shrinkage can affect many behaviors related to self-control, and can, in conjunction with the hippocampus, further affect memory and information recall. 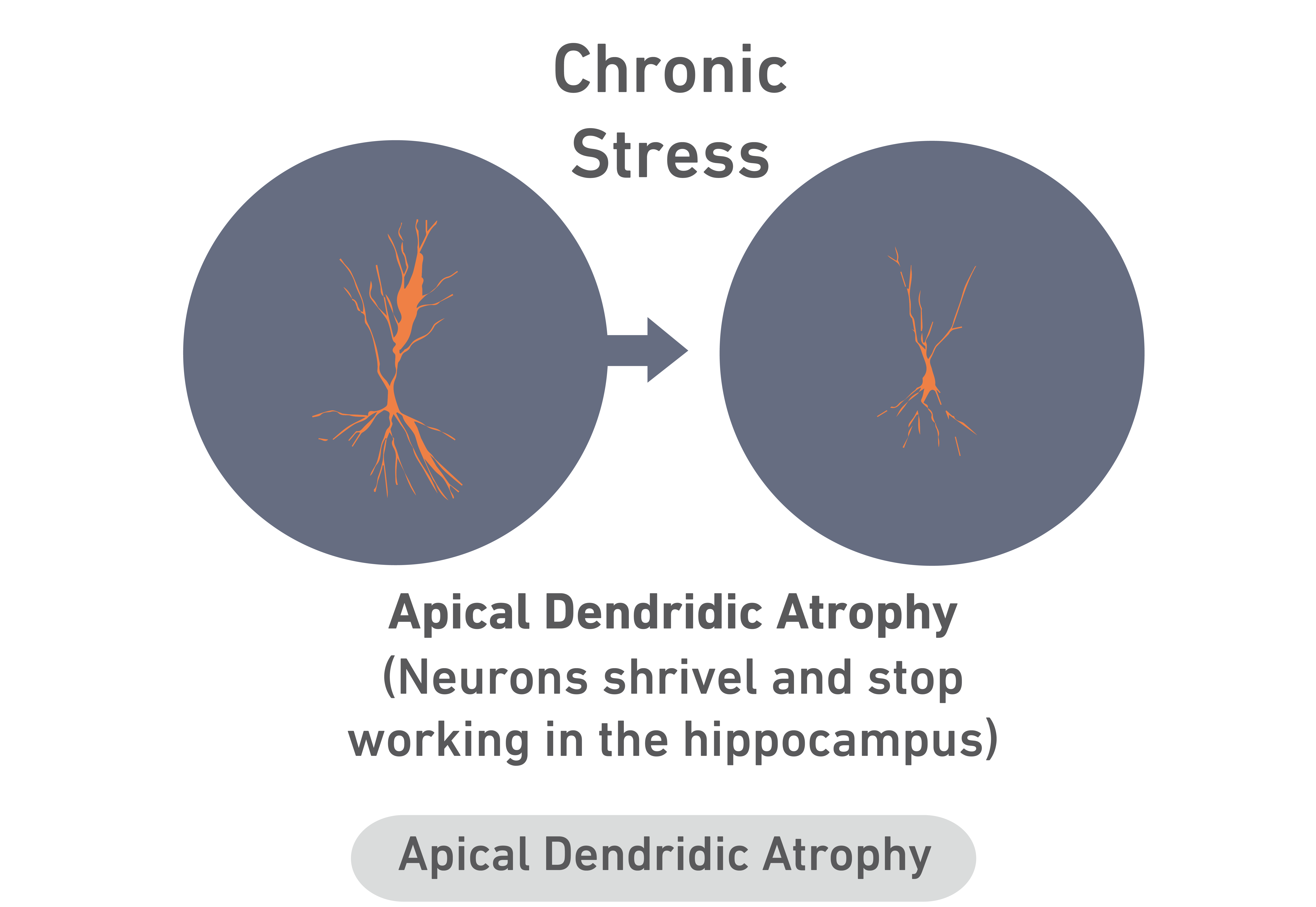
Additionally, hyperactive stress hormones reduce the firing of neurons in the prefrontal cortex, thus reducing the prefrontal cortex’s ability to communicate with the amygdala, hippocampus, and other regions of the brain. In other words, chronic stress prevents communication on pathways connecting the prefrontal cortex to other areas of the brain, thus preventing your normal or usual responses to different situations.
The prefrontal cortex does not shut down during chronic stress. However, the communication between the prefrontal cortex and other brain regions involved in the stress response is strained.
The connection between the elephant and the rider is strained.
In times of stress, all of the body’s systems coordinate to keep you alive. This means that over time, processes and functions not necessary for survival may turn down or turn off. The body will change. Thoughts will change. You may forget things, or remember strange and seemingly random pieces of information. Simply, your body and brain prioritize your survival over your short-term health, your personality, and your happiness.
To survive, you need to be alert and attentive to threats. You do not need to recall a recipe. Or to smile.
As stress mounts, the body and the brain will abandon certain functions, even change shape and size, in order to sustain you and protect you. On one hand, this is an incredible feat, and it is fascinating to see how our bodies work to protect us from harm.
At the same time, we are more than our bodies. We are more than survival. As stress increases and the brain and body change to keep you alive many of the changes will be emotionally painful, even scary.
In the context of chronic stress, you may feel like you are losing key parts of who you are. You may feel like you are losing your sense of self. While terrifying, this is normal, and there are ways to claim it back.